Cystic fibrosis and the impacts of limited NHS funding
- Neil Sardesai

- Oct 26, 2019
- 4 min read
Updated: Nov 8, 2020
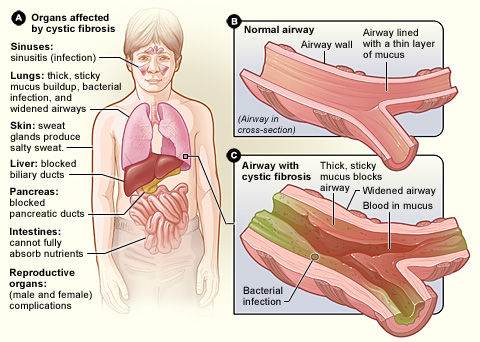
Cystic fibrosis is an inherited, genetic condition affecting 1 in 2,500 babies born in the UK. Due to mutations in the CFTR gene, the CFTR protein stops working correctly, resulting in chloride ions not being moved to the cell surface membrane. Without chloride ions on the surface of the cells, water is not attracted to those cell surfaces resulting in the mucus becoming thicker and more sticky. This exacerbates the build-up of mucus in the lungs and digestive system. This clogs up the bronchi, causing bacteria and dust particles to get trapped in the the airways. This often results in infection, inflammation and respiratory failure. Sadly, it is also a progressive disease, meaning that its symptom get worse as the person ages
In the UK, every baby has the option of receiving a blood spot test, also known as a heel prick test, at around five days old. As part of this test, 4 drops of blood are collected from the baby's heel and placed on a special card. This allows for immediate screening for 9 different rare genetic conditions, including sickle cell anaemia, congenital hypothyroidism and cystic fibrosis. As such, treatment can immediately begin, such as providing a high-energy diet, medicines and physiotherapy.

The main risk associated with cystic fibrosis is to do with the lungs. This is because, as explained above, the sticky mucus builds up causing difficulty breathing and lung infections. The mucus can also affect the pancreas as it stops enzymes such as amylase and lipase reaching food in the digestive system. As such, the breakdown of this food is much slower, meaning that people suffering from cystic fibrosis must eat more calories to account for that. Victims of cystic fibrosis also suffer from many other associated symptoms including chest infections, coughing and jaundice. Cystic fibrosis can also lead to further complications as it increases the risk of other conditions such as diabetes, liver problems and osteoporosis (brittle bone disease).
In addition to the heel prick test, cystic fibrosis can also be tested for using a sweat test. In this test, the salt content of the person's sweat is measured (as a person who has cystic fibrosis will have a much higher salt content in their sweat). A genetic test can also be used to check a person's genes for the presence of the faulty gene.
Cystic fibrosis is a recessive disease. As such, both the mother and the father need to pass on the faulty, recessive gene to their child for the child to suffer from cystic fibrosis. Because the disease is recessive, the parents do not have to suffer from the condition for their children to be sufferers - the parents just have to be carriers for the disease. As such, the genetic test above is also sometimes used on both parents before birth to check whether either parent is a carrier, thus predicting the chance of the baby having cystic fibrosis. This has led to some controversy as, while this test does reduce the number of children born with cystic fibrosis thus reducing financial and social strain on the parents and society as a whole, critics argue that this is the first step towards designer children and restricting diversity.
Unfortunately, currently, there is no cure for cystic fibrosis however lifestyle choices can reduce the impact of the symptoms. These include regular physical activity to help clear mucus from the lungs and improve overall health, as well as airway clearance techniques.
Eating properly is also essential, with dietitians advisings sufferers to eat extra calories, take vitamin and mineral supplements as well as taking digestive enzyme capsules. These capsules help replace the enzymes lost (as the pancreas often doesn't work properly) thus allowing more nutrients from food to be absorbed.
There are also several medicines available to help control or even reduce the symptoms of cystic fibrosis. These include antibiotics to help treat chest infections, mucus-thinning medication and bronchodilators. Further, as of November 2019, a new life-extending drug called Orkambi which improves lung function, thus reducing breathing difficulties, will be available on the NHS in England.
Orkambi is an example of both the advantages and the disadvantages that a public system gives in regards to drug pricing. On the one hand, due to reduced funding, the NHS can't afford some drugs and also has to limit the number of very expensive drugs it funds. Furthermore, as NHS Scotland and NHS England are slightly different institutions, some drugs are only available in one jurisdiction and not the other.
Nevertheless, there are several advantages in terms of drug pricing by having a fully public NHS. This is because, as there is only one institution providing medicines to the UK, the NHS has huge purchasing power, allowing them to seek lower prices. In the United States, individual hospitals buy their own medicines thus meaning that drug companies have less of an incentive to reduce the prices. In stark contrast, in the UK, the NHS buys medicines for the whole country. As such, drug companies are incentivised to lower prices since, if they don't, they don't have access to the entire UK market. This was the case with the drug Orkambi, whose owners originally wanted to charge £100,000 per patient per year before the price was drastically reduced.
These new developments in treating cystic fibrosis are incredibly important. At the moment cystic fibrosis affects about 10,400 people in the UK. Because of this negotiation, 5000 children in England will now be able to access this drug and hopefully gain a higher quality of life.
Sources:



Comments